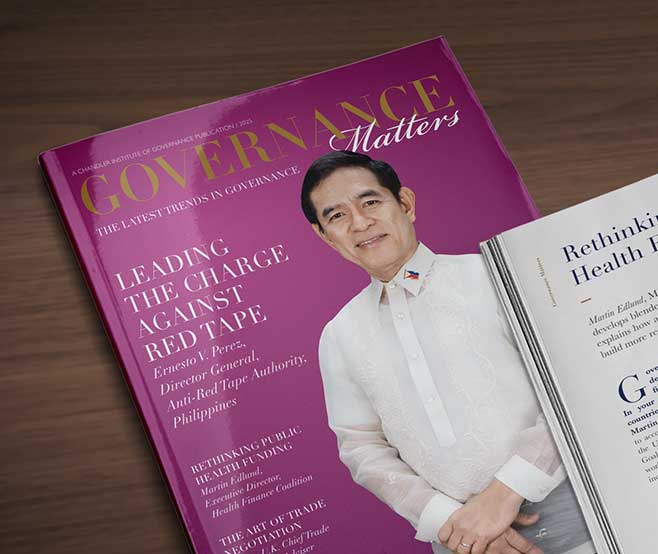
Delivering Universal Healthcare Effectively
Beverly Ho, Director of the Philippines Health Promotion Bureau, tells Governance Matters how the pandemic became a once-in-a-lifetime opportunity to accelerate healthcare reform by galvanising disparate stakeholders into action.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Heading 6
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
Governance Matters: What led you into healthcare? And how has your experience of working in that field changed your perspective?
Beverley Ho: I wanted to be a doctor because my mum was a doctor and I always believed it was a noble profession. When I entered public medical school, I saw that a lack of good primary care meant patients were arriving at very late stages of illness. It made me question how we could have the best minds working in medicine but still they were unable to make things work for people.
The lesson was that in the Philippines the quality of care is determined not by the doctors but by the quality of the system. The system we are working in needs to be fixed so that those who want to help can help and those that need help get help. These insights taught me that I could do most good not on the front line but at the back end, engineering the space for effective healthcare.
Now, through my role as the Director of the Health Promotion Bureau and the Disease Prevention and Control Bureau, I can make a real difference.
The Philippines passed a Universal Health Care (UHC) law in 2019. How has that helped to improve the system?
One of the critical things about the UHC Act was that it re-emphasised the role of the Department of Health, which in the Philippines is more of an enabler than a service provider. Back in 1991, when we devolved health services to local government units, there was a struggle within the Department of Health as some thought we should have kept a centralised system.
As a result of this institutional confusion, processes and support were not designed properly for a devolved setup. The UHC law has started the process of fixing this by strengthening the mandate for devolution. This has included the introduction of an explicit roadmap for reaching universal health care coverage and a more systematic means of gauging where the issues are. It has also strengthened the role of primary care and prioritised health promotion. This is a huge step change.
It forms what we call a local health system maturity model. Rather than focusing narrowly on the health programmes or on certain health indicators, we are taking a broader view of helping provincial systems mature. To achieve that, we have two jobs to do. First, to put the right standards in place, and second, to develop the tools to help them achieve those standards.
Among the tools we have developed are a series of playbooks to help local government units implement their health goals. These are essentially a series of templates, from a communications plan through to budget guides, which are intended to be a friendly tool for implementation on the ground. Working with civil society organisations, we have designed them for seven areas, covering things such as environmental health, mental health, violence, and injury prevention.
How did COVID-19 affect your work and inform the direction the Department of Health is taking towards health promotion and disease prevention?
The pandemic actually opened doors for us in the Health Promotion Bureau because, finally, there was more funding where there was very little before and we also had a huge boost in attention. A big chunk of the work in health promotion is dealing with other sectors. Normally that means knocking on doors and trying to encourage other agencies to work with us. In a pandemic, the reverse happened.
Now that those relationships are in place, the real work has started. We want to dispel the notion that health promotion equals communication. It is not just about educating people about wearing masks or the benefits of vaccines. We need a more holistic view of what good health entails.
As for disease prevention, for a long time, public health aficionados have emphasised primary care but never received much support. In the early days of the pandemic, the focus was indeed all on hospitals. Later on, though, people saw that we could not roll out vaccines efficiently because many people did not really have a relationship with their primary care provider. Our primary care system was not set up.
In my past 12 years of work, never have I heard so many people talk about primary care. We need to capitalise on that. The challenge within the Department of Health is to dismantle the silo mentality where many programme managers working on specific areas of health think of primary care as having nothing to do with them.

You work with a large range of stakeholders. How do you engage and work with government organisations, businesses, and citizens to deliver objectives?
There are two types of engagement with stakeholders, passive and active. During the pandemic, we had more passive engagement as huge numbers of partners approached us wanting to work with us. The challenge then was to avoid getting overwhelmed, which we managed by having a clear framework for working and knowing where we could find extra support.
In certain cases, we did not have enough resources, or were slowed by our procurement process so we needed to find help. This happened once when we were trying to produce a television advert and in the end, a funding body — Junior Chamber International, a rotary-style organisation — helped search for an advertising agency that could do it for free while we paid for the air-time. In other cases, people come to us offering support. For example, a public relations agency may offer to approach their clients to help place our health measures during a campaign. That has happened before and ended with our health messages being placed on the social media platforms of commercial entities to boost outreach. How we go about these sorts of partnerships really depends on what the objective is.
Do you think laws such as the tax on tobacco or sugar-sweetened beverages can help to advance the country’s healthcare goals? What is your experience of using such tools to promote public health?
Studies have demonstrated that these taxes have a real effect. First, you are lowering the consumption of something that is harmful, and second, those tax receipts can be earmarked, at least partially, for improving health services.
Our office is also responsible for other policies such as issuing and updating graphic health warnings or policies on, for example, active transport, working with the transportation sector to create new standards for safe, bike-friendly roads.
The Philippines’ National Economic and Development Authority (NEDA) and other organisations have been anticipating that the Philippines would achieve upper-middle income status sooner had it not been interrupted by the pandemic. When that happens, do you expect healthcare priorities to shift?
Economic empowerment will definitely be accompanied by a greater demand for choice. People will want universal healthcare but on their own terms — for example, an air-conditioned hospital room with their preferred doctor. As it is now, our country’s universal healthcare model limits choice (of accommodation, of physician, of brand of medicines) to enable “free” services.

Unfortunately, what we currently have is a two-tier healthcare system. I anticipate, and hope, that UHC reforms will narrow the gap between those two tiers but when we reach middle income status, there is going to be more pressure for divergence. Our challenge is to make sure that the Government has more levers in place by then.
There is a harmful notion that it is fine to let those who can afford it pay for themselves and just let the Government take care of the poor. However, studies continuously show that what happens in one tier affects what happens in the other. The level of regulation will probably have to improve when the country achieves middle income status. That goes back to having better government capacity.
How should health sector policymakers approach healthcare reforms to ensure successful delivery?

Maybe if you had asked me this question years ago, I would say to go as fast as you can, because it is very difficult to generate and sustain consensus. With years of experience, I would agree with the African proverb that, “If you want to go fast, go alone; but if you want to go far, go together.” More than ever in recent times, I have really seen the power of partnerships and coalition building.
Yes, the UHC law has been a huge improvement in our legislation. However, operationalising it is taking time, in part because not everyone is on board and lots of people are still just trying to understand what it means. Getting people to dream together, to imagine together, and to give them the fuel to work constructively together is the surest route to success.

Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Endnotes
- Item 1
- Item 2
- Item 3


Beverly Lorraine Ho is the Director of the Health Promotion Bureau and Disease Prevention and Control Bureau, which implements policies, programmes, and activities to address social determinants of health and creates supportive environments. She is concurrently the Director for the Control Bureau at the Department of Health, leading efforts to strengthen primary care and integrating service delivery of various public health programmes. She is a Fellow of the Maurice Greenberg World Fellows Program at Yale University, U.S.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.