From Ebola to COVID-19
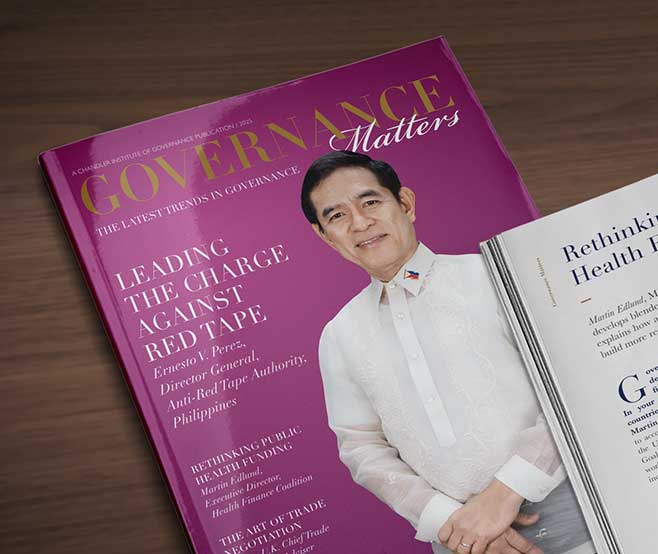
S. Olasford Wiah, Community Health Services Director for Liberia’s Ministry of Health, and Brittney Varpilah, Deputy Liberia Country Director at Last Mile Health, share how the lessons learned from the Ebola epidemic have contributed to a more robust national health system in Liberia that has been leveraged to respond to the COVID-19 pandemic.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Heading 6
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
From Ebola to COVID-19
As Liberia’s primary health system withstands another wave of COVID-19 infections in the country, community health workers such as Jerome Gardiner, continue to serve on the frontlines of the response. At the start of the pandemic, Gardiner and his peers were trained to recognise the signs and symptoms of COVID-19, encourage social distancing, hand washing, and mask use, and refer any suspected cases for treatment. They also employed no-touch protocols so that community health workers can stay safe while continuing to administer essential health services.
Gardiner and his fellow community health workers were already in place, serving their neighbours in rural and remote communities across Liberia, as part of a healthcare network that rose to tackle a former crisis: the West African Ebola epidemic.

A Historic National Community Health Worker Programme
However, a bright spot of the Ebola response was the engagement of communities across the country. Community members, including Gardiner, answered the call to serve when the government of Liberia asked for support in educating communities, tracing contacts, and rapidly referring patients to care in remote and rural areas. Although nationally, Liberia experienced a three-times decrease in facility-based delivery during the Ebola outbreak, facility-based delivery remained high in Konobo District, where paid and supervised community health workers kept providing services, dropping a mere three percent.
The government of Liberia recognised the urgent need to strengthen the health system, and the opportunity to leverage the power of the community. However, building a national health system that reached every last child and family across the country was an extraordinary challenge that required funding, research, expertise, and strong management. The only way to address such a challenge was in collaboration with partners.
In July 2016, six months after West Africa was finally declared Ebola-free, Liberia’s Ministry of Health assembled a powerful coalition of non-governmental organisations and donors (including the Clinton Health Access Initiative, International Rescue Committee, Last Mile Health, Partners In Health, Plan International), and funding partners (including USAID, Global Financing Facility, The World Bank, The Global Fund), and leading philanthropists to launch the National Community Health Assistant Program. The programme saw the deployment of a paid, professionalised community health worker — trained to deliver primary care, supervised by a registered nurse, and equipped with critical supplies — to every rural and remote community in the country.
Since then, the government and its partners have recruited, trained, supervised, equipped, and deployed more than 3,800 paid community and frontline health workers. These efforts to rebuild Liberia’s national primary health system demonstrate how NGOs and funders can support governments to achieve systemic change.
Today, more than 80% of Liberia’s community health workforce has been deployed nationwide. Community health workers have conducted more than 6.3 million patient home visits, and have delivered over 1.8 million treatments and screenings to children under five. In communities served by the national programme in Liberia, community health workers now treat 45% of all reported malaria cases for children under five. Just as importantly, they have kept primary health services going during the COVID-19 pandemic.

The Power of Partnership to Expand Primary Healthcare to All
The continued success of this programme — that aims to fully scale across the country in 2022 and be sustained over the long term — is fuelled by the power of partnership.
It started with a vision and framework laid out by the government of Liberia. The government asked its long-standing partners to align with its unified vision for a community health workforce capable of providing universal access to primary healthcare. The government called for collaboration amongst partners, and pushed non-governmental organisations and donors to shift from focusing on their own vertical or geographic-focused programming to making strategic investments in the government-led, community-based primary health system.
The investments by partners in Liberia’s vision of health for all have taken many forms. We would like to highlight a few here:
Evidence
Funding
Technical Assistance
First, the government of Liberia benefited from local evidence on the potential impact of community health worker programmes when it was planning its national programme. Last Mile Health and the Ministry of Health worked together in Konobo District of Grand Gedeh County to jointly identify problems, brainstorm solutions, and implement innovations to improve access to and the quality of healthcare being provided by a pilot community health worker program. This pilot allowed the Ministry of Health to test approaches, demonstrate effectiveness, measure impact and cost, and then build a foundation for national scale.
While funding may seem like an obvious way to partner, even here, Liberia offers an interesting lesson. One challenge the government of Liberia faced when advocating for this programme was shifting donors’ mindset on cost. Liberia is a low-income country that relies heavily on foreign assistance. Donors believed supporting the recurring costs of this programme — such as salaries for community and frontline health workers — was too costly and difficult, and made the programme unsustainable for Liberia. To support its vision of paid and professional community health workers, the government of Liberia cited evidence-driven, global best practices — which have since been institutionalised in the World Health Organisation’s guidelines on health policy and system support to optimise community health worker programmes. In addition, this vision was supported by a growing body of evidence that demonstrates that investing in quality, community-based primary healthcare that can meet up to 90% of a population’s health needs is the most equitable and efficient way to accelerate universal health coverage.
Based on this evidence, the Ministry of Health was able to build a coalition of donors and partners who were willing to work together and invest in the government’s vision. That vision, the National Community Health Assistant Program, would make strategic investments in building stronger health systems over the long run rather than focusing on less impactful and lower-cost quick fixes. Since then, Co-Impact, a global collaborative focused on systems change, unlocked additional financing for this programme to support its scale-up across the remaining rural areas and promote sustainability. The programme aims to reduce under-five child mortality by 20%, and eventually serve as a partnership-driven model for other countries looking to build or strengthen their community-based primary healthcare system.
And, finally, the Ministry of Health leveraged non-governmental organisations to lead initial programme implementation and management with a focus on building local capacity. With this phased approach, as county-level government capacity strengthens, organisations, role shift from lead implementers to embedded technical assistance providers. Eventually, the community health worker programme will transition to being fully managed and owned by the government. This approach of working in close collaboration with its partners allowed Liberia to expedite the implementation of the programme.
The Road Ahead: The Importance of Resilient Health Systems
The Ebola outbreak and the COVID-19 pandemic have both underscored the vital importance of resilient health systems that can reach all. Together with our partners, we look forward to fully scaling and sustaining the National Community Health Assistant Programme to reach every rural and remote community, advance universal health coverage, and protect against future disease threats.

Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Endnotes
1. https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=LR
2,3. Dahn, Bernice. Foreword to Liberia: Investment Case for Reproductive, Maternal, New-Born, Child, and Adolescent Health 2016-2020.
- Item 1
- Item 2
- Item 3


S. Olasford Wiah is the Director for the Community Health Services Division for the Liberia Ministry of Health. In this role, he oversees the country’s National Community Health Assistant Programme, which aims to provide universal access to primary healthcare for rural Liberians. The programme relies on paid and professional community health workers. Previously, Wiah served as the Community Health Department Director in River Gee County, where he contributed to the development of the national community health policy and program. He has a deep commitment to strengthening the primary healthcare system to achieve universal health coverage for all Liberians. He graduated as a Physician Assistant from the Tubman National Institute of Medical Arts in Liberia in 2009.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.

Brittney Varpilah is the Director of National Community Health Systems at Last Mile Health, an organisation that partners with governments to design, scale, strengthen, and sustain high-quality community health systems, which empower teams of community and frontline health workers to bring life-saving primary healthcare to the world’s most remote communities. In this role, she supports the Liberia Ministry of Health to scale and sustain the National Community Health Assistant Programme across all 15 counties to provide 1.2 million rural people with access to primary healthcare. She joined Last Mile Health in 2016 to support the development of the 2016-2021 Community Health Policy and the design of the accompanying curriculum for the national programme. Prior to joining Last Mile Health, she worked for Mercy Corps and World Learning. She holds a Master of Arts in International Education from SIT Graduate Institute.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.